Laboratory

Making Every Cycle Count
Some cases are so complex that even after a complete diagnosis and ensuring the embryo is of good quality, implantation failures occur. In such instances, we need to study the endometrium more thoroughly, as it plays a crucial role in embryo implantation.
Explore our additional tests for these cases:
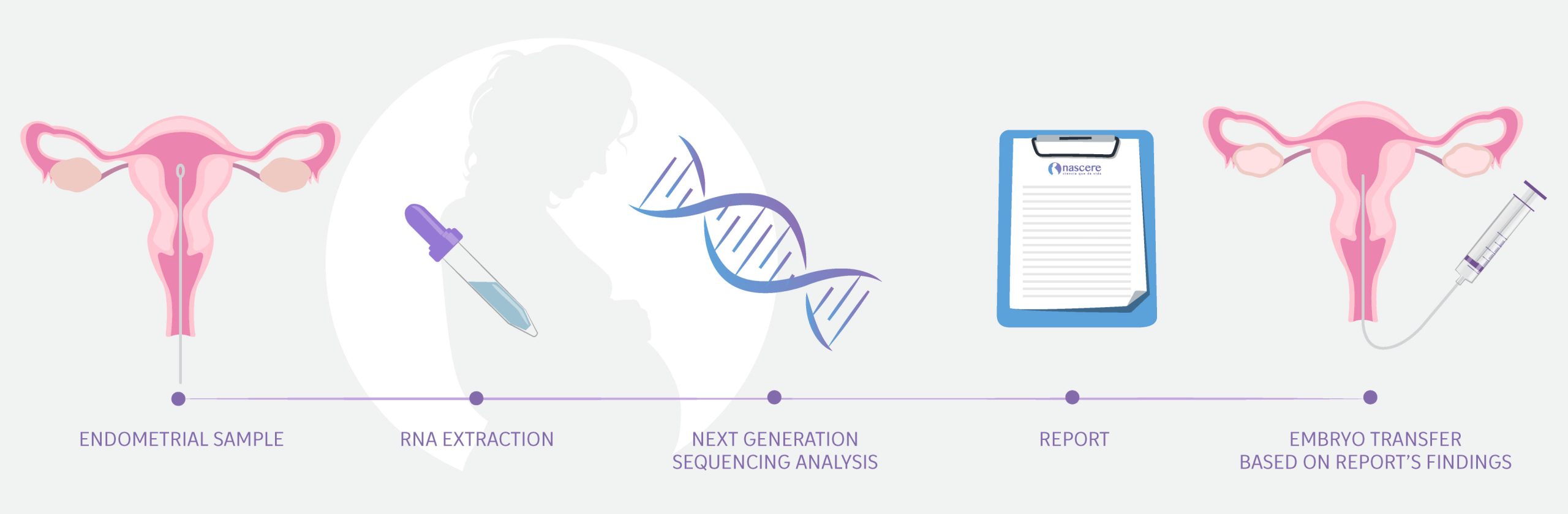
ERA: Endometrial Receptivity Analysis
When an IVF cycle fails despite optimal embryo quality, we need to study endometrial receptivity.
What is Endometrial Receptivity?
A receptive endometrium is one that is ready to receive the embryo. This occurs during a specific period called the implantation window, which is unique to each woman.
Understanding and being able to precisely calculate this implantation window helps improve pregnancy chances, as we can coordinate embryo transfer according to the best days for each patient.
ERA helps identify the implantation window for patients with previous implantation failures.
EMMA+ALICE
This test aims to evaluate your endometrial flora and detect if you have endometritis. Since we are pursuing two different goals, the evaluation consists of two parts.
Part 1: EMMA – Endometrial Microbiome Metagenomic Analysis
When an IVF cycle fails despite optimal embryo quality, we need to study endometrial receptivity, including the endometrial flora.
What is Endometrial Flora?
The endometrial flora, or microbiome, refers to the microorganisms present in the endometrium. According to various studies, an unbalanced endometrial flora is associated with implantation failure.
EMMA helps us determine the percentage of healthy bacteria (lactobacillus) in your endometrium, allowing us to take action to balance them if necessary.
Part 2: ALICE – Analysis of Infectious Chronic Endometritis
As mentioned before implantation failures not attributable to embryo quality often require a closer examination of the endometrium.
One often overlooked condition is chronic endometritis, a continuous inflammation of the endometrium caused by pathogenic bacteria.
- ALICE detects the bacteria most frequently responsible for chronic endometritis, enabling us to start treatment for endometritis.
How is it done?
For both tests, we follow the same procedure:
Who is this test ideal for?
Remember, EMMA + ALICE is a two-part test conducted simultaneously, recommended for:
- Women with repeated pregnancy losses.
- Patients with repeated implantation failures in IVF.
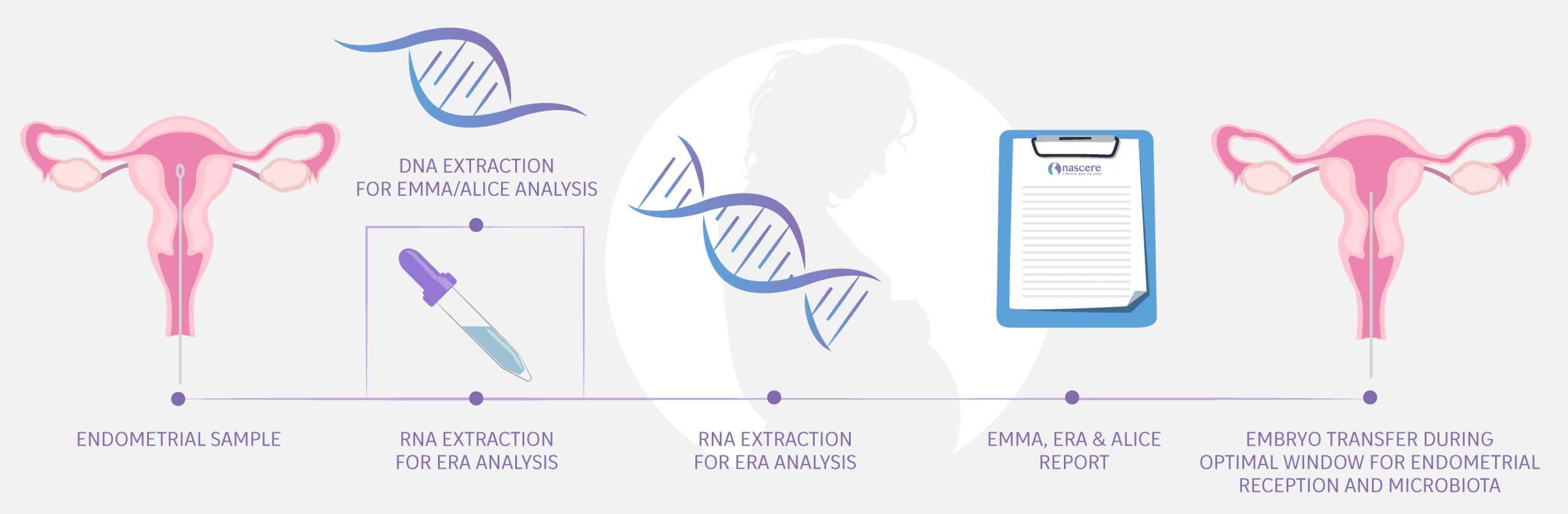
EndomeTRIO
Designed especially for patients who can take advantage of the benefits that ERA + EMMA + ALICE tests offer.
- ERA helps identify the implantation window when the endometrium is most receptive and ready to receive the embryo.
- EMMA helps us determine the percentage of healthy bacteria in your endometrium.
- ALICE detects the bacteria most frequently responsible for chronic endometritis.
Together, these tests ensure we make the most of each transfer cycle, increasing the probability of success.
How is it done?
HScope
To complete your diagnosis, in some cases, we need to perform a hysteroscopy, a procedure that allows us to physically examine the uterus and check the condition of the cervix, the inside of the uterus, and the fallopian tubes.
How is it done?
We insert a thin, flexible tube with a 3mm lens through the cervix to examine the uterine cavity.
When is it recommended?
When the cause of infertility cannot be visualized through other tests, such as radiological exams.
Direct Sperm Analysis (Seminogram)
Evaluating the male factor helps us cover all possible causes of infertility.
We do this through a direct sperm analysis or seminogram, which allows us to assess semen quality by considering the number of sperm per sample, their shape, and motility, as well as the pH of the seminal fluid, among other factors.
How is it done?
By providing us with a semen sample in a sterilized container that we provide at the clinic after a period of 2 to 7 days of sexual abstinence. The sample can be taken at NASCERE or at home, as long as you deliver it within 30 minutes after ejaculation.
Once you provide the sample, we take it to the Andrology laboratory where we perform tests established by the WHO.
Quality Parameters Established by WHO
According to the World Health Organization (WHO), we evaluate the following aspects:
- Licuefacción: Una muestra debe concluir su licuefacción a temperatura ambiente en un periodo de 15 a 20 minutos.
- Viscosidad: Se refiere a la fluidez de la muestra, que puede ser normal o alta. Si es alta, puede indicar disfunción prostática.
- Volumen: El volumen mínimo normal en un período de 3 a 5 días de abstinencia es de 1.4 ml.
- Color: El semen es de color blaquecino opaco, ligeramente amarillento. Si presenta algún otro, se debe buscar la causa.
- pH: El valor debe estar por encima de 7.1.
- Concentración: El valor normal es de 15 millones por cada 1ml de eyaculado
- o 39 millones en la totalidad de la muestra.
- Motilidad: El porcentaje de espermatozoides móviles que se desplazan debe superar el 32%.
- Morfología: El 4% o más de espermatozoides deben ser de constitución normal.
- Vitalidad: Se refiere al porcentaje de espermatozoides vivos y debe superar el 58%
What if the necessary parameters are not met?
We will investigate the cause for not meeting the parameters. In some cases, we may provide recommendations or medical treatments to correct the issue, or we will explore additional tools offered by Assisted Reproduction to support you.